USC scientists create living drug to fight cancer and HIV
Team L&M
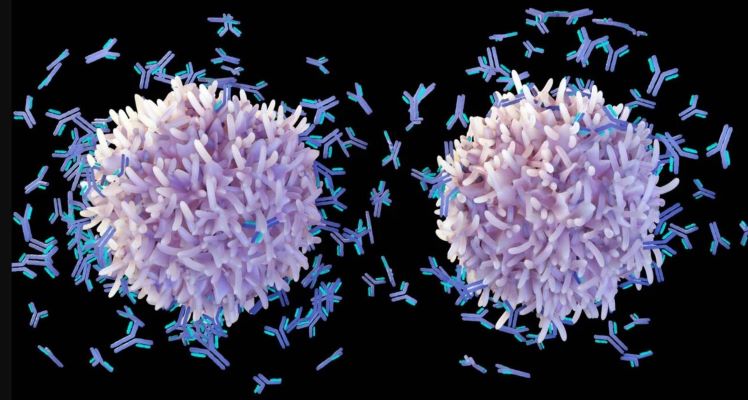
Scientists from the University of Southern California (USC) have discovered a way to turn the body’s B cells into tiny surveillance machines and antibody factories that can pump out specially designed antibodies to destroy cancer cells or HIV, two of medicine’s most formidable foes.
The research, published in Nature Biomedical Engineering, describes a technique for editing the genes of immune cells called B cells, turbocharging them to fight even the sneakiest invaders. The work is an important advance in harnessing the power of antibodies to treat conditions ranging from Alzheimer’s disease to arthritis.
“In some diseases or conditions, the natural antibodies made by B cells are just not good enough,” said senior author Paula Cannon, a Distinguished Professor of Molecular Microbiology & Immunology at the Keck School of Medicine of USC. “HIV is a very good example of that. It mutates constantly, keeping one step ahead of whichever antibodies are being thrown at it. We thought a checkmate move might be persuading B cells to make an antibody that was so broad in its ability to ‘see’ HIV that HIV couldn’t easily mutate around it.”
The beauty of the technique, the researchers said, is it can be adapted to produce a broad range of different antibodies.
“It’s a technology for reprogramming B cells that could be applied to almost anything you can imagine dealing with an antibody,” said first author Geoffrey Rogers, a research associate and senior postdoctoral fellow in Cannon’s lab. “We think we’ll be able to completely customize everything about the antibody.”
For this project, the researchers took inspiration from chimeric antigen receptor (CAR) T cells, “living drugs” designed to target specific things. They’ve revolutionized treatment for blood cancers like leukemia and lymphoma. With CAR T treatment, T cells — sister cells to B cells — are removed from a patient’s blood and genetically modified to identify cancer cells by recognizing a marker on their surface. Millions of the cells are then infused into the patient’s body, where they fight disease and then fade away.
How B cells behave
B cells behave differently, making them more suitable for fighting chronic conditions. They function as both a security system and antibody factory, residing long-term in the bone marrow, lymph nodes and spleen — and firing up when needed.
To make these tiny fighters, Cannon and Rogers used CRISPR gene editing methods to place the instructions for custom antibodies at the exact site in the B cell’s DNA where antibodies are naturally made. This trick means that B cells can be reprogrammed as biofactories making the custom antibodies. And just as regular antibodies respond to vaccination, the reprogrammed B cells could also be stimulated to increase their output.
Researchers were able to observe the antibodies at work using tonsil tissue to replicate an immune system in a dish.
The researchers are working with the USC Stevens Center for Innovation to license the technology for commercial use. The USC Stevens Center helps scientists shepherd their discoveries from the lab to the market.
“We’re really excited to help try and bring this to biotech companies,” said Erin Overstreet, executive director of the USC Stevens Center. “This could be a fundamental shift in how we approach certain diseases.”

